Introduction
Welcome to Peak Performance Physical Therapy’s educational reference on epidural steriod injections.
 Epidural steroid injections (ESI) are commonly used to control back and leg pain from many different causes. These injections control pain by reducing inflammation and swelling. They do not fully cure any of the injuries they are commonly used for, but they can control the symptoms for prolonged periods of time. In many cases, the ESI is used to control the symptoms so that you can participate in a physical therapy program, become more active, and be better able to control your chronic symptoms.
Epidural steroid injections (ESI) are commonly used to control back and leg pain from many different causes. These injections control pain by reducing inflammation and swelling. They do not fully cure any of the injuries they are commonly used for, but they can control the symptoms for prolonged periods of time. In many cases, the ESI is used to control the symptoms so that you can participate in a physical therapy program, become more active, and be better able to control your chronic symptoms.
This guide will help you understand:
- where the injection is given
- what your doctor hopes to achieve
- what you need to do to prepare
- what might go wrong
- what Peak Performance Physical Therapy’s approach to rehabilitation is
Anatomy
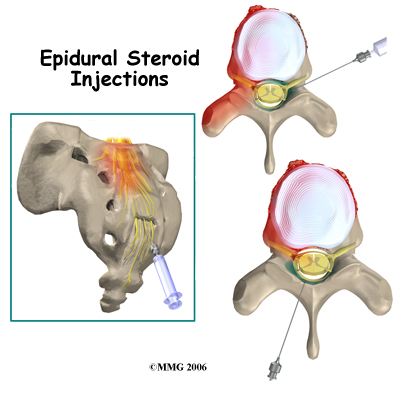
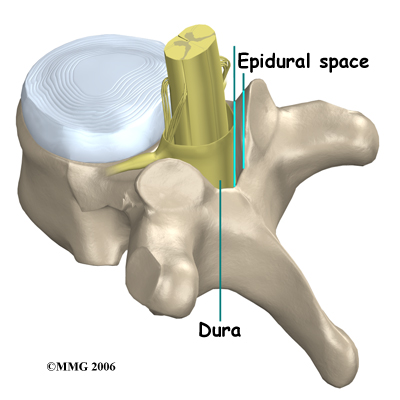
What parts of the body are involved?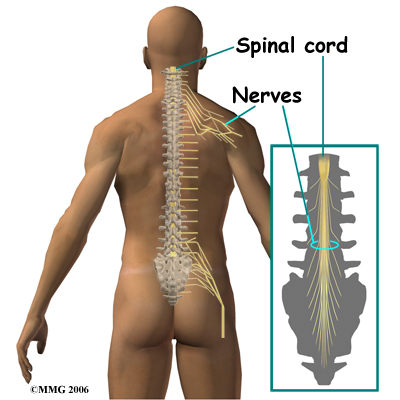 When doing an ESI, the doctor inserts a needle through the skin so that the tip of the needle is in the epidural space. This space is the area between the bony ring of the spine and the covering of the spine called the dura. The dura is the sac that encloses the spinal fluid and nerves of the spine. In the cervical spine and thoracic spine, the whole length of the spinal cord is also contained within the dura and the spinal sac. In the lumbar spine the spinal cord actually stops at the second lumbar vertebra but the nerves continue on. This means that in the lower lumbar spine there are only spinal nerves running within the spinal sac.
When doing an ESI, the doctor inserts a needle through the skin so that the tip of the needle is in the epidural space. This space is the area between the bony ring of the spine and the covering of the spine called the dura. The dura is the sac that encloses the spinal fluid and nerves of the spine. In the cervical spine and thoracic spine, the whole length of the spinal cord is also contained within the dura and the spinal sac. In the lumbar spine the spinal cord actually stops at the second lumbar vertebra but the nerves continue on. This means that in the lower lumbar spine there are only spinal nerves running within the spinal sac.
The epidural space is normally filled with fat and blood vessels. Fluid such as the lidocaine and cortisone that is injected during an ESI is free to flow up and down the spine and inside the epidural space to coat the nerves that run inside the spinal canal.
There are several openings in the bones that surround the epidural space where a needle can be placed. When doing an ESI, the needle is placed in one of three of these openings. Each of these three types of ESI injections has its specific advantages.
Related Document: Peak Performance Physical Therapy's Guide to Lumbar Spine Anatomy
An interlaminar injection is performed by placing the needle directly in from the back of the spine between the lamina of two adjacent vertebra. The laminae (plural) form the outer rim of the bony ring of the vertebra. This places the tip of the needle in the back side of the spine. The advantage to this type of injection is that it is easy to do, even without the guidance of a special type of x-ray machine, called a fluoroscope. The injection is usually done between the two vertebra that are most likely causing your pain. This puts the medications as close as possible to the problem. The disadvantage to this type of injection is that injected medication may stay in the back side of the spine away from the intervertebral disc.
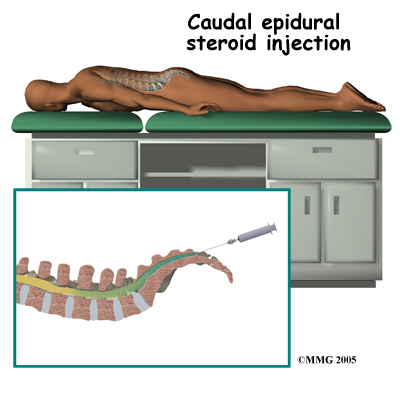 A caudal injection is also relatively easy to perform even without x-ray guidance. The caudal injection is performed at the very lower end of the spine through a small opening in the bones of the sacrum. The sacrum is made up of several vertebrae that fuse together during development to form a single large bone. This large bone is situated where the pelvis connects to the spine. The opening at the tip of the sacrum leads directly to the epidural space. Fluid injected through this opening can flow upward through the epidural space to coat the nerves throughout the lower lumbar spine.
A caudal injection is also relatively easy to perform even without x-ray guidance. The caudal injection is performed at the very lower end of the spine through a small opening in the bones of the sacrum. The sacrum is made up of several vertebrae that fuse together during development to form a single large bone. This large bone is situated where the pelvis connects to the spine. The opening at the tip of the sacrum leads directly to the epidural space. Fluid injected through this opening can flow upward through the epidural space to coat the nerves throughout the lower lumbar spine.A transforaminal injection is a newer type of injection that is done from the side of the spine, through the neural foramen. The neural foramen is the opening where the nerve root exits the spine. There are two neural foramen between each vertebrae, one on each side.
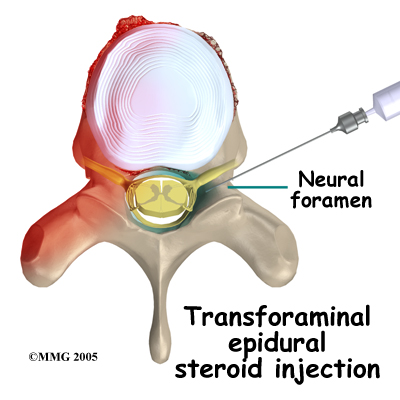
The doctor places the tip of the needle into the neural foramen using the fluoroscopic x-ray machine to watch and guide the needle into the correct position. The advantage to this type of injection is that it places the medication in the front of the spinal canal, near the intervertebral disc. The disadvantage is that this type of injection definitely requires the use of the fluoroscopic x-ray to guide the needle placement.
Rationale
What does my doctor hope to achieve?
Your doctor is recommending an ESI to try and reduce your pain. The ESI may also reduce numbness and weakness. During an ESI the medications that are normally injected include an anesthetic and cortisone. An anesthetic medication (such as novacaine, lidocaine or bupivicaine) is the same medication that is used to numb an area when you are having dental work or having a laceration sutured. The medication causes temporary numbness lasting one to six hours, depending on which type of anesthetic is used.
Cortisone is an extremely powerful anti-inflammatory medication. When this medication is injected around inflamed swollen nerves and connective tissues, it can reduce the inflammation and swelling. Reducing the inflammation reduces pain. Reducing swelling can allow the nerves to function better, which in turn can reduce numbness and weakness.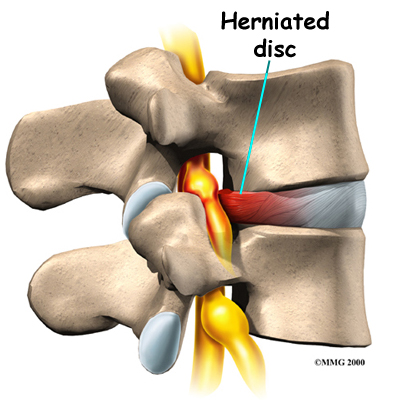 ESI injections are temporary and may last from a couple of weeks to a couple of months. They may be used to reduce your symptoms so that you can more easily begin a physical therapy program with less pain. They may also be used to reduce symptoms and let the body repair the underlying condition. For example, most disc herniations cause a great deal of pain, particularly when they first occur. This is due to the chemicals that leak from the torn disc and inflame the nerves. Over several weeks to months, the disc heals enough to stop leaking these chemicals. If the cortisone can reduce the symptoms at the beginning, then when the cortisone injection wears off, the chemical irritation may be gone and the pain may not return. It should be noted that the cortisone itself does not heal the damage to the disc herniation itself.
ESI injections are temporary and may last from a couple of weeks to a couple of months. They may be used to reduce your symptoms so that you can more easily begin a physical therapy program with less pain. They may also be used to reduce symptoms and let the body repair the underlying condition. For example, most disc herniations cause a great deal of pain, particularly when they first occur. This is due to the chemicals that leak from the torn disc and inflame the nerves. Over several weeks to months, the disc heals enough to stop leaking these chemicals. If the cortisone can reduce the symptoms at the beginning, then when the cortisone injection wears off, the chemical irritation may be gone and the pain may not return. It should be noted that the cortisone itself does not heal the damage to the disc herniation itself.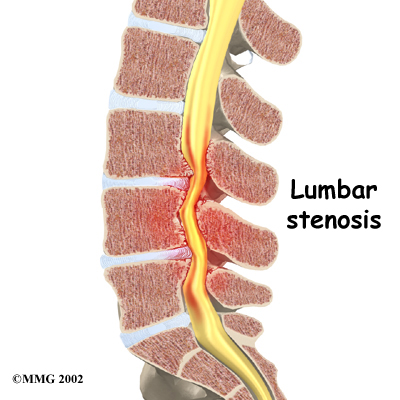
In other conditions, the cortisone injection is repeated 1 to 3 times per year to help control symptoms. This is usually recommended when surgery is too risky or when you choose not to have surgery. For example, in older adults with spinal stenosis, this may be an alternative less risky treatment compared to other options. Spinal stenosis occurs when the spinal canal where the nerves travel is too tight. This results in inflammation and swelling of the nerves and soft tissues. The swelling makes the spinal canal even tighter. The nerves do not have enough room to function correctly and they begin to cause pain, numbness and weakness. An ESI once every six months may reduce the swelling enough to reduce the pressure on the nerves as well as the symptoms of pain, numbness and weakness.
One question that always comes up is "How many ESIs can I have?" There is no definite answer to that question. Most doctors would recommend that you limit the number of injections to 3-5 per year. The limit is not to the number of injections into the body but rather to the amount of cortisone put in your body. Cortisone has bad side effects seen in your bones, skin and other areas when you take or use the medication too often in either a cream format, pill format or as an injection. Due to these side effects, doctors do not like to do these injections more often than necessary.
Preparations
How will I prepare for the procedure?
Your doctor may tell you to be "NPO" for a certain amount of time before the procedure. This means that you should not eat or drink anything for the specified amount of time before your procedure. This means no water, no coffee, no tea or anything. If you take regular medications you may receive special instructions to take your medications with a small amount of water. Check with your doctor if you are unsure of what to do.
You should tell your doctor if you are taking any medications that "thin" your blood or interfere with blood clotting. Other medications also slow down blood clotting. Aspirin, ibuprofen and nearly all of the anti-inflammatory medications affect blood clotting, as do medications used to prevent strokes. These medications usually need to be stopped 7 days prior to the injection. Be sure to let your doctor know if you are on any of these medications.
Procedure
What happens during the procedure?
When you are ready to have the ESI, you will be taken into the procedure area and an IV will be started. The IV allows the nurse or doctor to give you any medications that may be needed during the procedure. The IV is also for safety because it allows a very rapid response if you have a problem during the procedure, such as an allergic reaction to any of the medications injected. If you are in pain or anxious, you may also be given medications through the IV for sedation during the procedure.
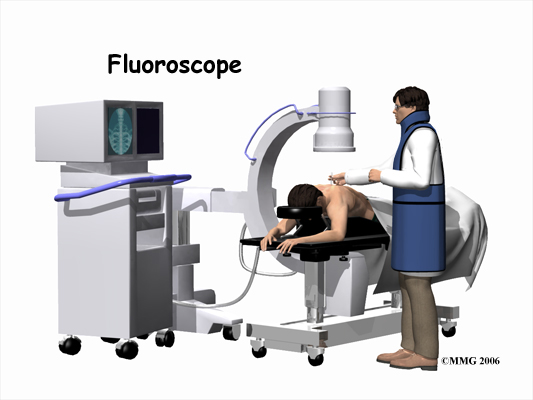
Despite the ability to do some ESI procedures without fluoroscopic guidance, most ESI procedures today are done with the help of the fluoroscopy machine. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure. This allows the doctor to watch where the needle goes as it is inserted, which makes the injection much safer and much more accurate. Once the needle is in the right location, a small amount of radiographic dye is injected. This liquid dye shows up on the x-ray image and the doctor can watch where it goes. The anesthetic medication and the cortisone will go in the same place, so the doctor wants to make sure that the injection will put the medication in the right place to provide the most benefit. Once the correct position is confirmed, the anesthetic and cortisone are injected and the needle is removed.
When the procedure is over you will then be taken out of the procedure room to the recovery area. You will remain in the recovery area until the nurse is sure that you are stable and that you have not had any allergic reaction to the medications. The anesthetic may cause some temporary numbness and weakness. You will be free to go when these symptoms have resolved.
After Care
What happens after the procedure?
You will be able to go home soon after the procedure, probably within one hour. If all went as planned, you probably won't have any restrictions on activity or diet.
Most doctors will arrange a follow up appointment, or phone consult, within one or two weeks after the ESI to see how you are doing and to determine what effect the procedure has had on your symptoms.
You can return to physical therapy immediately.
Rehabilitation after ESI
Unless your doctor recommends otherwise, physical therapy at Peak Performance Physical Therapy after ESI can begin immediately.
As indicated above, the ESI is done to try and reduce your pain. The pain in your back, however, can be from a variety of different injuries therefore the rehabilitation treatment you receive at Peak Performance Physical Therapy will vary according to what structures are involved in causing your back pain, and your treatment will also be tailored to suit your specific individual needs.
Some aspects of general rehabilitation, however, will be similar for all back pain patients who have undergone an ESI. It is important to use any window of time where your back pain has decreased or has been eliminated as a result of the ESI to engage in rehabilitation. Often this pain-free or pain-reduced time allows you a window where you can more effectively rehabilitate your back and improve your overall movements.
During your first few treatments your therapist will initially work to relieve any residual pain that you may have following the ESI. They may use heat, ice, or electrical modalities such as ultrasound or interferential current to help decrease your pain. They may also massage around your back, buttocks, and hip areas to provide relief by relaxing tight muscles that are pulling on the joints of the back.
In order to know how best to treat your individual back problem, your physical therapist will assess your back and will determine how well your back is moving as well as determine if you have any muscular imbalances affecting your back. They will also take note of any other symptoms you feel such as tingling or numbness and will test for any muscle weakness that may be present in your low back or legs. If it is determined that the movement in your back is limited, your therapist will work to encourage more motion. In order to do this they may use joint mobilizations or manipulations, performing passive stretching, and massage any tight muscles related to the area. Stretches and strengthening exercises as part of a home program will also be prescribed as they can help you gain more motion in your own back, improve the strength and endurance of the muscles that help to support your back, and work to correct any muscle imbalances that may exist. These exercises will be targeted at your low back directly, but may also include exercises for your abdominals and trunk (core) area, buttocks and hips, groin, and the front and back of your thighs.
Maintaining a strong core muscle area is the most crucial part of managing your back pain and allowing you to maintain as active of a lifestyle as you can despite any chronic pain. Your physical therapist can teach you how to properly activate the core muscles and build up their strength and endurance. Even just simple exercises such as gently tightening the muscles of your deep abdominal area directly after you have undergone your injection will help to support your back. If your therapist has assessed your back and deemed it to be relatively moving too much, then the core exercises prescribed are even more crucial. Stretching exercises that target the tight muscles, which may be pulling your back into an adverse position, will also be prescribed. As you improve your activation, strength, and endurance of your core muscles, more advanced exercises will be prescribed in order to challenge the ability of these muscles and ensure they can stabilize the spine during everyday functional activities.
Another area particularly important in helping to support your back is your hip/buttocks (gluteal) area. Your therapist will assess both the range of motion of your hips as well as the ability of your gluteal muscles to support your hips and back. If your hip range of motion is poor or your gluteals are not strong enough then extra stress is transferred to your low back. Again, often that short window of time after your ESI where you may have less pain is a useful period where you can more effectively strengthen your buttocks muscles. The flexibility of the anterior hip muscles as well as the muscles of the front and back of your thigh will also be assessed and stretches may be provided if any of these muscles are found to be tight or overactive.
Doing your prescribed exercises in a hydrotherapy pool may be a useful option for you that you can discuss with your therapist. Often the warmth of the pool and the hydrostatic properties of the water can make range or motion, strengthening, and overall retraining of muscular control easier.
As with any injury or biomechanical dysfunction, maintaining one’s posture and alignment is very important. Despite whether your therapist determines that your low back has increased or decreased motion, they will be strict in encouraging you to maintain proper posturing and alignment at all times. Maintaining good posture can significantly decrease the stress put through the back. Any window of time that you have which is pain-free after your injection can also be particularly useful in re-training your body to maintain proper alignment. By improving the endurance of the muscles that support your back, you will be able to maintain your posture and alignment for longer periods of time, and lengthen the time frame between any flare-ups that may occur.
In addition to your posture your gait will also be reviewed. Pain in your back can not only affect your static posture but can also cause you to develop an inefficient walking pattern that puts unnecessary stress on the joints in your lower extremities and your back. In a normal day most people take thousands of steps just to get around therefore an inefficient or improper walking pattern can quickly lead to further pain in the back itself or can cause pain in other related joints. Your physical therapist will assess your gait and ensure that you are walking properly.
Your therapist may also suggest the use of tape or a back brace in order to help manage your back pain and encourage proper posturing and alignment. Tape can be a useful method to assist the muscles to support your back. A brace can help to support your back long-term particularly during prolonged static or active periods. Sometimes a trial of tape before an expensive brace is purchased is a good method of determining the potential use of a brace. Your physical therapist can discuss whether or not they feel a brace would be useful in your individual case.
Once your back pain is under control your therapist will discuss the importance of a cardiovascular program to assist in managing your back pain long-term. At Peak Performance Physical Therapy we believe that maintaining your overall fitness level is an effective method in helping to manage both the pain and stress that comes with chronic pain and also helps to decrease the number of flare-ups that occur. Your therapist can discuss with you the best cardiovascular activity options that would be appropriate in your individual case. Often cycling, water aerobics, water running, or other low impact activities are the most appropriate ones to begin with when starting cardiovascular activity after an epidural injection.
Generally the treatment we provide at Peak Performance Physical Therapy for your back after an ESI can assist greatly in managing your back pain but it should be remembered that these injections are not generally a cure for your chronic pain; they are only a part of your overall pain management plan. You will need to continue working long- term with your doctor, physical therapist, and any other health care professional involved in your pain management. You will also need to continue faithfully doing your rehabilitation home program in order to best manage your pain. If your pain is ongoing despite the injection and regular physical therapy treatment your doctor may want to discuss the possibility of another injection or other pain management options.
Peak Performance Physical Therapy provides services for physical therapy in Baton Rouge.
Complications
What might go wrong?
There are several complications that may occur during or after the procedure. The ESI procedure is safe and unlikely to result in a complication, but no procedure is 100% foolproof. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Complications are uncommon, but you should know what to watch for if they occur. 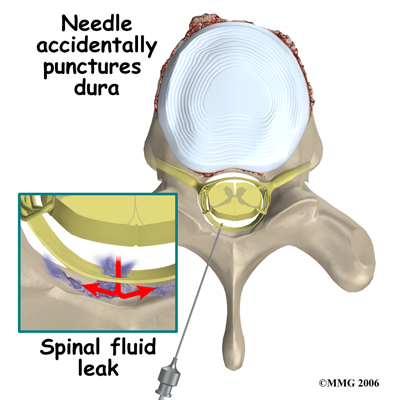 Probably the most common complication of an ESI is what is called a wet tap. This occurs when the needle penetrates the spinal sac and enters the spinal fluid. This is the same thing that happens when your doctor performs a spinal tap or a spinal anesthetic. In itself, it is not dangerous, however, because the epidural needle is larger than the spinal needle, the hole in the spinal sack may continue to leak and not seal itself off immediately which causes a spinal fluid leak, or what is termed a wet tap. This spinal leak causes a very bad headache, which is worse when you are sitting or standing upright and may cause nausea and vomiting. The headache occurs because the spinal fluid pressure in the skull decreases. A key symptom is that the headache goes away if you lie flat or with your head a bit lower than your feet because in these positions the spinal fluid pressure in your skull goes back to normal. Most spinal headaches go away on their own in a few days when the hole in the spinal sac heals naturally and closes. You may be instructed to stay flat for a couple of days until this occurs.
Probably the most common complication of an ESI is what is called a wet tap. This occurs when the needle penetrates the spinal sac and enters the spinal fluid. This is the same thing that happens when your doctor performs a spinal tap or a spinal anesthetic. In itself, it is not dangerous, however, because the epidural needle is larger than the spinal needle, the hole in the spinal sack may continue to leak and not seal itself off immediately which causes a spinal fluid leak, or what is termed a wet tap. This spinal leak causes a very bad headache, which is worse when you are sitting or standing upright and may cause nausea and vomiting. The headache occurs because the spinal fluid pressure in the skull decreases. A key symptom is that the headache goes away if you lie flat or with your head a bit lower than your feet because in these positions the spinal fluid pressure in your skull goes back to normal. Most spinal headaches go away on their own in a few days when the hole in the spinal sac heals naturally and closes. You may be instructed to stay flat for a couple of days until this occurs.
There are also ways, however, to speed up the healing of the puncture in the spinal sac. The most common treatment is to do a blood patch. If the doctor sees that the spinal sac has been punctured before he removes the needle, this may be done at the time of the ESI. If it is not done at the time of the injection then this procedure may be done several days later if the headache has not gone away, which indicates that the hole has not healed on its own. A blood patch procedure involves taking a small amount of blood from a vein in your arm and injecting it into your back in the epidural space. The blood clots and "patches" the hole.
There are several other possible complications of the ESI. These include infection, epidural abscess, epidural hematoma, and nerve damage.
Any time a needle is inserted through the skin, there is a possibility of infection. Before any invasive procedure is done, the skin is cleansed with a disinfectant and the health care provider doing the procedure uses what is called a sterile technique. This means that the instruments and the area where the skin is punctured remains untouched by anything that is not sterile. The doctor will also use sterile gloves and proper hand washing techniques to reduce the overall chance of an infection.
Signs of an infection are increasing redness, swelling, pain, and a fever. Almost all infections will need to be treated with antibiotics. An epidural abscess is when an infection occurs inside the spinal canal. The infection can cause a large pocket of pus to form around the nerves, which again puts too much pressure on the nerves and causes symptoms. An epidural abscess will probably require surgery to correct or improve and antibiotics will also be necessary to treat the infection.
An epidural hematoma occurs when one of the small blood vessels around the spinal sac continues to bleed after the procedure. The bleeding can cause a large pocket of blood to form around the nerves, which puts too much pressure on the nerves and causes symptoms. An epidural hematoma will also likely require surgery in order to treat.
Finally, because the injection is done inside the spinal canal, the spinal nerves can be damaged by the needle itself. This usually will recover and will not require any additional procedures to correct.
Portions of this document copyright MMG, LLC
